Category: Myoclonus
Objective: We report the first known case of a patient with refractory post-hypoxic myoclonus (PHM) and focal epilepsy implanted with bilateral subthalamic nuclei (STN) deep brain stimulation (DBS).
Background: Chronic PHM also known as Lance-Adams Syndrome (LAS) is a neurologic complication of cardiopulmonary arrest that can result in action and stimulus myoclonus that can be refractory to medications [1,2]. There are a handful of these refractory cases that have been successfully treated with DBS in the Globus Pallidus interna (GPi) or the thalamus [3-9].
Method: Case Report
Results: We present a 38-year-old man with no pertinent past medical or family history who presented after a fall from a horse and subsequent cardiopulmonary arrest with return of spontaneous circulation after one round of cardiopulmonary resuscitation. He developed cortical multifocal myoclonus within the days following the accident concerning for LAS. He later developed right hemispheric focal epilepsy. Medications controlled his seizures, but refractory myoclonus prevented him from returning to work. Extensive work-up to localize his epilepsy and myoclonus determined that both his focal seizures and myoclonus originated from the right more than left sensorimotor cortices. Given these findings and discussion between movement disorders and epilepsy, the decision was made to implant the bilateral STN. Escalation of his stimulation resulted in neuropsychiatric side effects including irritability, emotional lability, impulsivity, mania, and inattention likely related to medio-ventral spreading of the stimulation. Stimulation of the most dorsal contacts improved, but did not eliminate, these side effects.
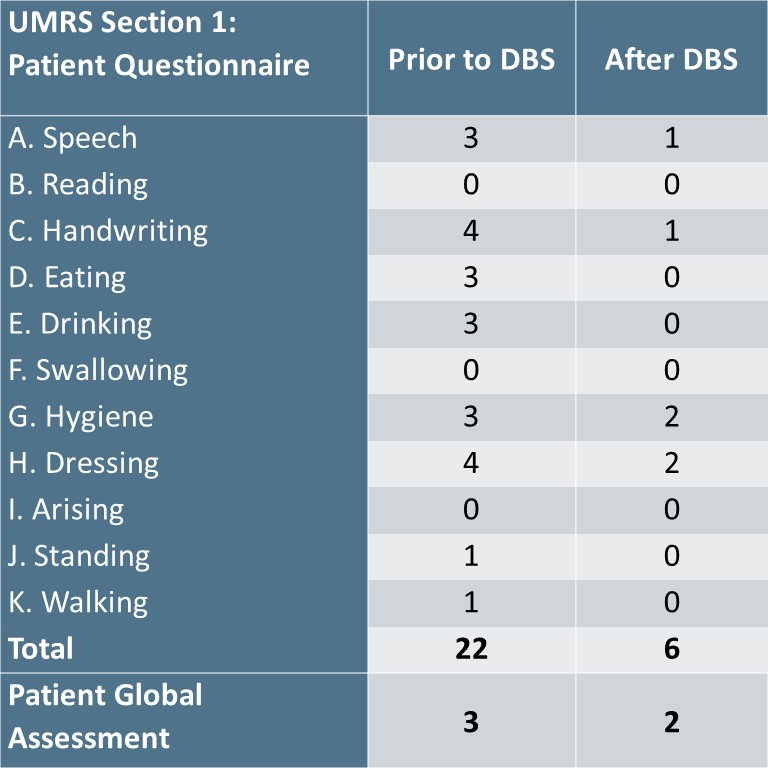
Within these limitations of stimulation, there was no objective difference in the patient’s myoclonus ON stimulation and after 1 hour OFF stimulation using the Unified Myoclonus Rating Scale (UMRS). This may have been caused by inadequate washout time or concurrent use of medications on the morning of the visit. Retrospectively, however, he reported a 73% subjective improvement on Section 1 of the UMRS when comparing his symptoms before and after DBS [table 1].
Conclusion: Based on our experience and the available literature, STN might be a potential DBS target to consider for medication refractory LAS. However, more research, including improvement in objective measurements, is needed.
Table 1: UMRS Section 1 Scores
References: 1. Freund B, Kaplan PW. Post-hypoxic myoclonus: Differentiating benign and malignant etiologies in diagnosis and prognosis. Clin Neurophysiol Pract. 2017;2:98-102. doi:10.1016/j.cnp.2017.03.003
2. Lance JW, Adams RD. THE SYNDROME OF INTENTION OR ACTION MYOCLONUS AS A SEQUEL TO HYPOXIC ENCEPHALOPATHY1.; 1963. https://academic.oup.com/brain/article/86/1/111/263353
3. Ramdhani RA, Frucht SJ, Kopell BH. Improvement of post-hypoxic myoclonus with bilateral pallidal deep brain stimulation: A case report and review of the literature. Tremor and Other Hyperkinetic Movements. 2017;7. doi:10.7916/D8NZ8DXP
4. Mure H, Toyoda N, Morigaki R, Fujita K, Takagi Y. Clinical Outcome and Intraoperative Neurophysiology of the Lance-Adams Syndrome Treated with Bilateral Deep Brain Stimulation of the Globus Pallidus Internus: A Case Report and Review of the Literature. Stereotact Funct Neurosurg. 2020;98(6):399-403. doi:10.1159/000509318
5. Asahi T, Kashiwazaki D, Dougu N, et al. Alleviation of myoclonus after bilateral pallidal deep brain stimulation for Lance–Adams syndrome. J Neurol. 2015;262(6):1581-1583. doi:10.1007/s00415-015-7748-x
6. Kim J, Inbo H, Kim HS, et al. First Clinical Report on the Treatment of Parkinson’s Disease with Fetal Midbrain Precursor Cells. Movement Disorders. Published online April 1, 2023. doi:10.1002/mds.29316
7. Gao F, Ostrem JL, Wang DD. Treatment of post-hypoxic myoclonus using pallidal deep brain stimulation placed using interventional MRI methods. Tremor and Other Hyperkinetic Movements. 2020;10:1-6. doi:10.5334/tohm.544
8. Öztürk G, Taşçı İ, Samanci MY, Peker S. Is deep brain stimulation useful in lance–adams syndrome? Neurol Asia. 2021;26(3):617-620. doi:10.54029/2021ykj
9. Kobayashi K, Katayama Y, Otaka T, et al. Thalamic deep brain stimulation for the treatment of action myoclonus caused by perinatal anoxia. Stereotact Funct Neurosurg. 2010;88(4):259-263. doi:10.1159/000315464
To cite this abstract in AMA style:
E. Tharp, J. Gavvala, M. Hafeez, S. Pati, S. Lhatoo, N. Tandon, R. Mehanna. Treatment of Post-hypoxic Myoclonus using Bilateral Subthalamic Nuclei Deep Brain Stimulation [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/treatment-of-post-hypoxic-myoclonus-using-bilateral-subthalamic-nuclei-deep-brain-stimulation/. Accessed July 10, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/treatment-of-post-hypoxic-myoclonus-using-bilateral-subthalamic-nuclei-deep-brain-stimulation/