Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To validate the self-completed version of the International Movement Disorder Society – Non-Motor Rating Scale (MDS-NMS)1, named the MDS-NMS – Questionnaire (MDS-NMS-Q).
Background: The MDS-NMS is a comprehensive 13-domain rating scale for assessing severity and frequency of non-motor symptoms (NMS) in Parkinson’s disease (PD), with a non-motor fluctuations (NMFs) subscale. The MDS-NMS is rater-completed, while the MDS-NMS-Q is a self-completed alternative assessing just symptom severity, with the globally-used NMSQuest as an exemplar2.
Method: Participants with a diagnosis of idiopathic PD first self-completed the MDS-NMS-Q unsupervised, and then were administered the MDS-NMS by a rater blinded to the MDS-NMS-Q results. A total of 175 participants completed the main scale for MDS-NMS-Q and MDS-NMS, and 78 completed the NMFs subscale for both instruments.
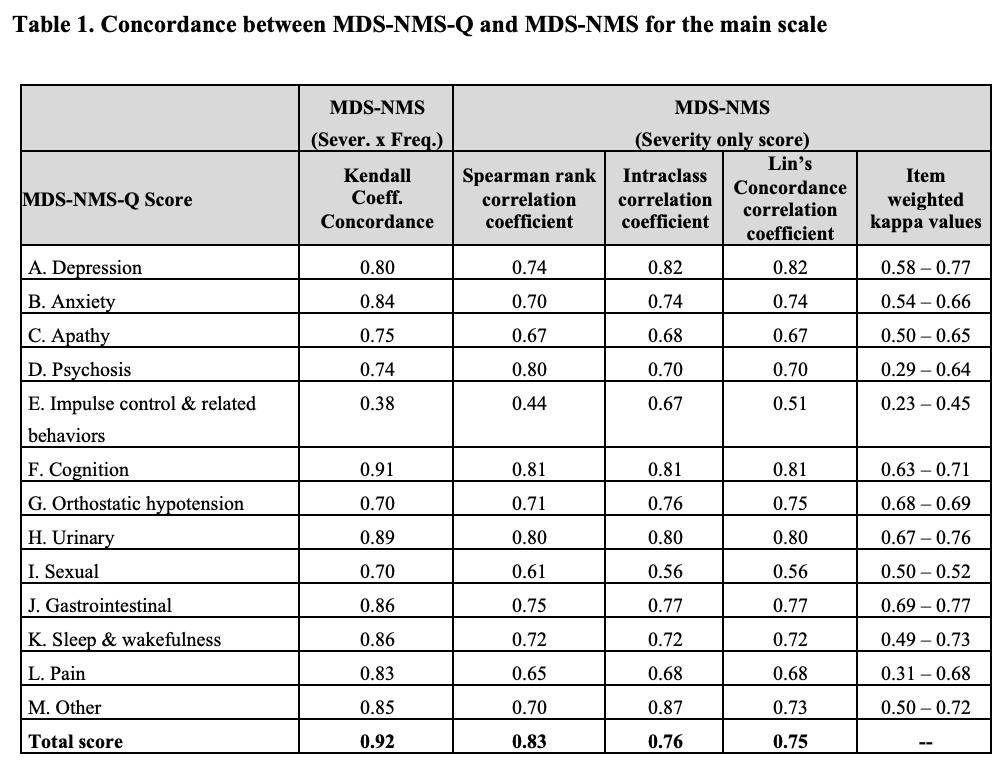
Results: The overall cohort was 62.6% male, with mean (SD) age 67.9 (10.4) and PD duration 9.0 (6.8) years. 91% were in Hoehn & Yahr stages 1-3. The mean (SD) MDS-NMS-Q score was 43.0 (35.3), with range 0-133. No floor or ceiling effect was observed for total MDS-NMS-Q score, but a floor effect (i.e., absence of symptom) was present for the majority of individual domains. The mean (SD) MDS-NMS-Q NMFs score for those reporting NMFs was 18.5 (18.7), with range 0-72. Kendall coefficient of concordance for MDS-NMS-Q and MDS-NMS domain scores ranged from 0.38 (Impulse control & related behaviors) to 0.89 (Urinary) and was 0.92 for the total score (Table 1); 1 domain had “fair” agreement (concordance 0.21-0.40), 5 domains had “good” agreement (concordance 0.41-0.60), and 7 had “very good” agreement (concordance 0.61-0.80). Spearman rank correlation coefficient for MDS-NMS-Q NMFs and MDS-NMS NMFs subscale items ranged from a low of 0.17 (bladder) to a high of 0.51 (cognition), and the Kendall coefficient of concordance for the total score was 0.74.
Conclusion: The main scale of the self-completed MDS-NMS-Q overall has good to very good agreement with rater-administered MDS-NMS at the domain level, indicating that self-completion is an acceptable alternative to rater administration. The concordance between the MDS-NMS-Q and the MDS-NMS for the NMFs subscale items is only slight to moderate, suggesting suboptimal performance for this component of the instrument.
Table 1
References: 1.Chaudhuri KR, Schrag A, Weintraub D, et al. The Movement Disorder Society Nonmotor Rating Scale: Initial validation study. Mov Disord. 2020;35(1):116-133.
2.Chaudhuri K, Martinez-Martin P, Schapira A, et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Movement Disorders. 2006;21:916-923.
To cite this abstract in AMA style:
D. Weintraub, KR. Chaudhuri, A. Schrag, P. Martinez-Martin, A. Rizos, E. Mamikonyan, J. Gallagher, J. Staunton, M. Pereira Fernandes, C. Rodriguez Blazquez. Validation of the International Parkinson and Movement Disorder Society – Non-Motor Symptoms – Questionnaire (MDS-NMS-Q) [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/validation-of-the-international-parkinson-and-movement-disorder-society-non-motor-symptoms-questionnaire-mds-nms-q/. Accessed July 5, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/validation-of-the-international-parkinson-and-movement-disorder-society-non-motor-symptoms-questionnaire-mds-nms-q/