Session Information
Date: Wednesday, June 22, 2016
Session Title: Cognitive disorders
Session Time: 12:00pm-1:30pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To compare the utility for detecting Mild Cognitive Impairment in Parkinson’s disease (PD-MCI) of three abbreviated global scales: the Montreal Cognitive Assessment (MoCA), the Parkinson’s disease-Cognitive Rating Scale (PD-CRS) and the Addenbrooke’s Cognitive Examination new version (ACE-III).
Background: The Movement Disorders Society (MDS) proposed guidelines for diagnosing PD-MCI including two assessment levels: abbreviated (Level-I) and comprehensive (Level-II). The availability of cognitive scales adapted to new MDS criteria with high discriminative abilities can improve the precision of PD-MCI identification in a clinical setting.
Methods: The study sample included early PD patients (≤5 years from diagnosis) with normal cognition (PD-NC) or PD-MCI based on Level-II MDS criteria (two tests within each cognitive domain). Receiver operator curve (ROC) analyses were generated to calculate the area under the curve (AUC) and to measure the sensitivity and specificity of the cutoff scores from the Level-I scales. To examine the utility as screening tools, the optimal cutoff was defined as the lowest value providing ≥80% sensitivity (SEN). To use them as diagnostic tools, the optimal cutoff was the highest value providing ≥80% specificity (SPE).
Results: After screening for inclusion criteria, 71 PD patients [53.5% males; age= 68.7 (10.0SD) years; education=11.5 (4.9SD) years; PD evolution= 2.0 (1.7SD) years] completed the assessment.
| Total (n=71) | PD-NC (n=51) | PD-MCI (n=20) | P value t-test (PD-NC vs PD-MCI) | |
| mean (SD) | mean (SD) | mean (SD) | ||
| Age (years) | 68.7 (10.0) | 66.9 (10.6) | 73.0 (6.7) | 0.006 |
| Gender, n Males (%) | 38 (53.5) | 29 (56.9) | 9 (45.0) | N.S |
| Education (years) | 11.5 (4.9) | 12.2 (4.4) | 9.7 (5.8) | N.S |
| PD Evolution (years) | 2.0 (1.7) | 1.9 (1.7) | 2.0 (1.8) | N.S |
| HADS Depression | 3.2 (3.1) | 3.1 (2.8) | 3.7 (3.8) | N.S |
| HADS Anxiety | 5.2 (4.1) | 5.5 (4.2) | 9.4 (7.4) | N.S |
| PD-CFRS | 1.7 (1.9) | 1.3 (1.8) | 2.8 (2.0) | 0.004 |
| Task (max) | PD-NC (n=51) | PD-MCI (n=20) | P value |
| MDS Level-I | mean (SD) | mean (SD) | |
| MoCA (30) | 25.9 (2.8) | 21.9 (3.2) | <0.001 |
| PD-CRS (134) | 94.8 (12.2) | 72.2 (9.0) | <0.001 |
| ACE-III (100) | 91.7 (6.8) | 80.0 (8.3) | <0.001 |
| MDS Level-II | |||
| Attention & WM | |||
| TMT-A (sg) | 52.2 (17.3) | 90.6 (32.3) | <0.001 |
| Digits Backward (max span) | 3.9 (0.9) | 2.9 (0.8) | <0.001 |
| Executive Function | |||
| TMT-B (sg) | 137.3 (69.1) | 341.1 (144.1) | <0.001 |
| Phonetic Fluency | 16.2 (4.3) | 10.9 (3.9) | <0.001 |
| Memory | |||
| FCSRT DFR | 9.6 (3.4) | 5.2 (3.1) | <0.001 |
| ROCF 30′ | 12.7 (6.7) | 5.1 (4.3) | <0.001 |
| Language | |||
| BNT | 54.5 (4.1) | 49.7 (4.7) | <0.001 |
| Semantic Fluency | 19.9 (5.7) | 13.8 (4.5) | <0.001 |
| Visuospatial Function | |||
| JLOT | 21.6 (4.8) | 16.4 (5.3) | <0.001 |
| VOSP Number Location | 8.1 (1.3) | 7.2 (2.5) | 0.07 N.S. |
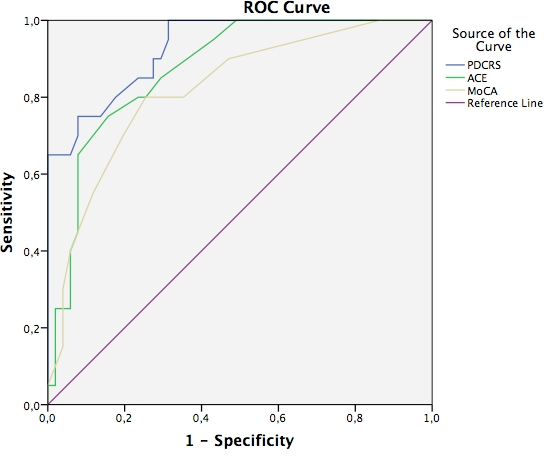
Conclusions: The PD-CRS shows the best performance as a diagnostic tool for PD-MCI, compared to the MoCA and the ACE-III results. These findings support the MDS recommendation allowing the application of an abbreviated assessment option to identify PD-MCI in non-demented PD patients.
To cite this abstract in AMA style:
R. Fernandez-Bobadilla, J. Pagonabarraga, J.A. Matias-Guiu, S. Martínez-Horta, A. Horta-Barba, J. Marin-Lahoz, J. Perez-Perez, B. Pascual-Sedano, H. Bejr-Kasem, A. Campolongo, J. Kulisevsky. Comparison of the utility of three cognitive scales for MDS Level-I diagnosis of mild cognitive impairment in Parkinson’s disease: MoCA, PD-CRS and ACE-III [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/comparison-of-the-utility-of-three-cognitive-scales-for-mds-level-i-diagnosis-of-mild-cognitive-impairment-in-parkinsons-disease-moca-pd-crs-and-ace-iii/. Accessed July 26, 2024.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/comparison-of-the-utility-of-three-cognitive-scales-for-mds-level-i-diagnosis-of-mild-cognitive-impairment-in-parkinsons-disease-moca-pd-crs-and-ace-iii/
