Category: Technology
Objective: In our previous work, we developed machine learning models to predict and detect freezing-of-gait (FOG) [1]. In this study, we aimed to use those models to inform a wearable FOG prevention device that cues the user only when FOG is identified, thereby reducing FOG time and improving gait.
Background: Cueing has been shown to help people with PD reduce FOG episode occurrence and severity [2]. However, rhythmic cues may worsen a person’s freezing if the cues are uncoordinated with the person’s walking. Also, people can get accustomed to rhythmic cueing and as a result, it loses effectiveness [3]. Cueing activated only when necessary may mitigate the risk of habituation and enhance its efficacy in alleviating FOG.
Method: We asked 20 participants to walk a freeze-inducing path 30 times with our FOG prevention device. Participants were also asked to return for another testing session in which we oversampled each participant’s data to generate personalized FOG prediction models. We also adjusted the device settings based on the results from the previous session. The prediction model used data from 21 previously tested participants to predict and detect FOG. The output was then used to activate a wearable sensory cue mechanism in real-time. The device was switched off before randomly selected trials which served as a control.
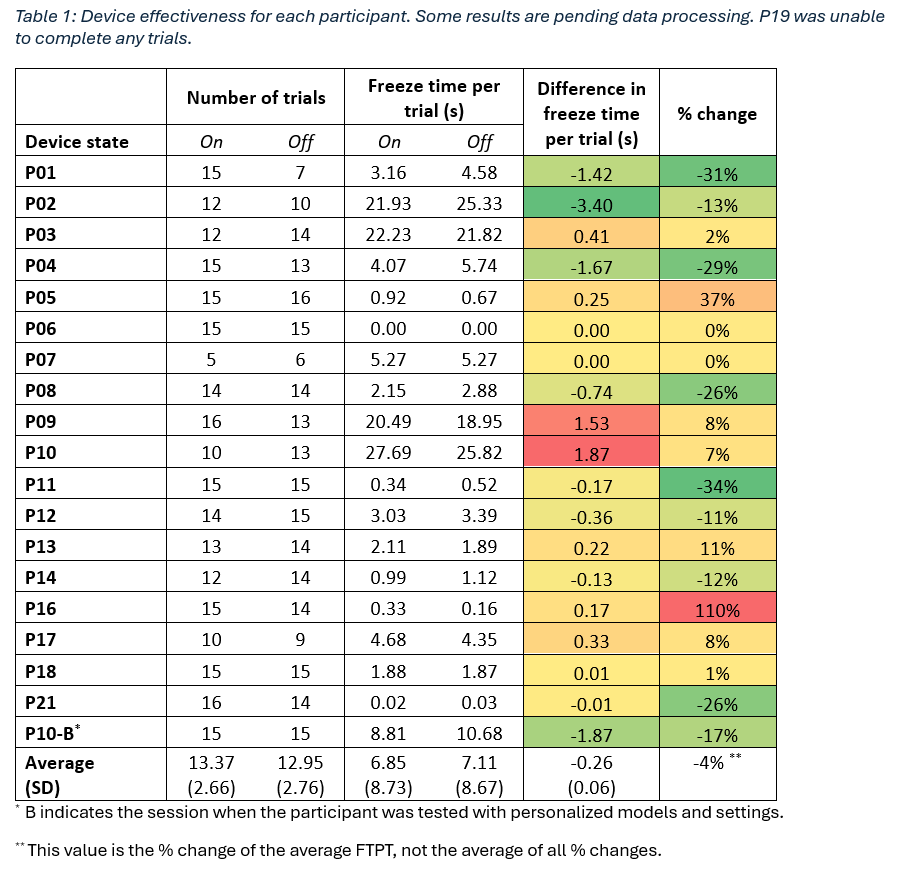
Results: Our preliminary results from 19 trials in [table 1] show that the device decreased FOG time for 8 participants, increased FOG time for 5 participants, and 5 participants were unaffected (<0.1s or <2% change in FOG time per trial). On average, all participants had a 0.37s (4%) decrease in freeze time per trial (FTPT). P01 had a 1.42s decrease in FTPT, 31% lower than their FTPT with the device off. P10 had a 1.87s (7%) increase in FTPT. However, when P10 was retested with personalized prediction models and device settings, they experienced a 1.87s (17%) decrease in FTPT.
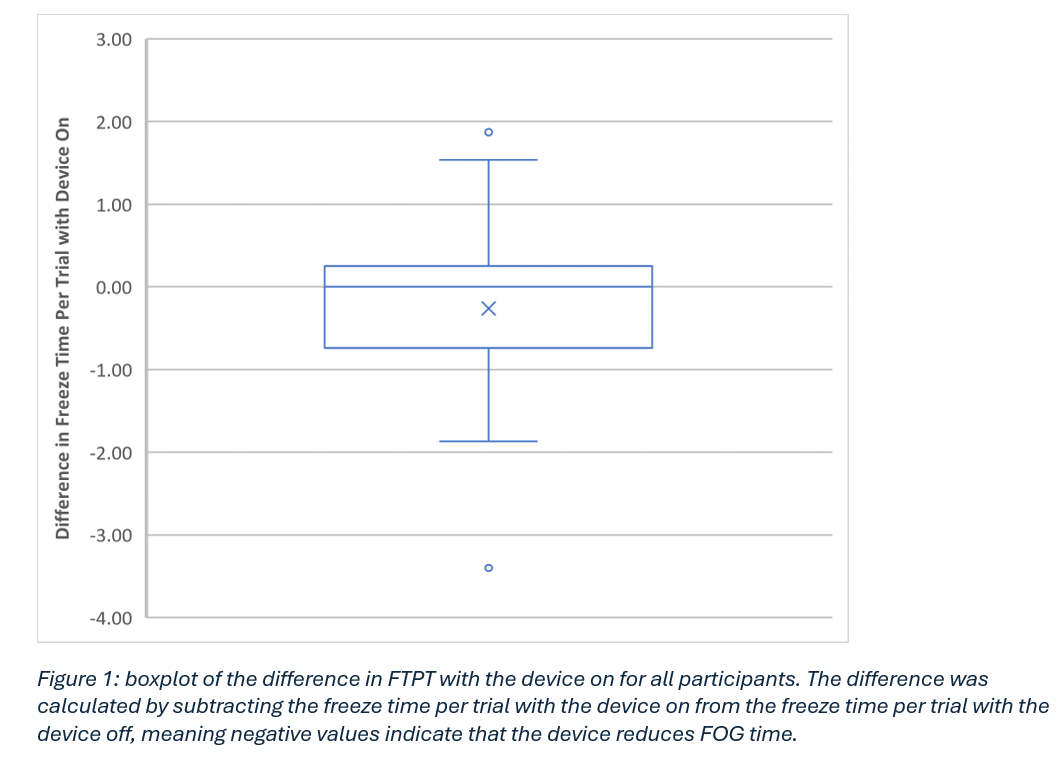
Conclusion: We found that the device performs well for some participants and on average slightly decreases FTPT as shown in [figure 1]. However, when one participant was tested with personalized settings and models, the device performance improved dramatically. This indicates that the personalization impacts device effectiveness significantly. Our results also show that this FOG prevention device can decrease FOG time, possibly reducing risk of falling and improving quality of life for people with PD who experience FOG.
Table 1
Figure 1
References: [1] S. Pardoel, J. Nantel, J. Kofman, and E. D. Lemaire, “Prediction of freezing of gait in Parkinson’s disease using unilateral and bilateral plantar-pressure data,” Front Neurol, vol. 13, Apr. 2022, doi: 10.3389/fneur.2022.831063.
[2] P. Ginis, E. Nackaerts, A. Nieuwboer, and E. Heremans, “Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-the-art and novel perspectives,” Annals of Physical and Rehabilitation Medicine, vol. 61, no. 6. Elsevier Masson SAS, pp. 407–413, Nov. 01, 2018. doi: 10.1016/j.rehab.2017.08.002.
[3] A. Nieuwboer, “Cueing for freezing of gait in patients with Parkinson’s disease: A rehabilitation perspective,” Movement Disorders, vol. 23, no. SUPPL. 2. 2008. doi: 10.1002/mds.21978.
To cite this abstract in AMA style:
A. Alakhras, S. Pardoel, E. Jafari, J. Kofman, E. Lemaire, J. Nantel. Wearable Device for Real-Time Prevention of Freezing-of-Gait in Parkinson’s Disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/wearable-device-for-real-time-prevention-of-freezing-of-gait-in-parkinsons-disease/. Accessed July 9, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/wearable-device-for-real-time-prevention-of-freezing-of-gait-in-parkinsons-disease/