Category: Parkinsonism, Atypical: MSA
Objective: To assess clinical and neuroimaging factors associated with survival in a cohort of patients with a final clinical diagnosis of Multiple System Atrophy (MSA) according to the MDS-MSA criteria.
Background: MSA is the synucleinopathy with the poorest survival. Several studies have described clinical factors associated with a higher risk of mortality in MSA patients 1–4. Less is known about the impact of FDG-PET findings on survival in MSA patients.
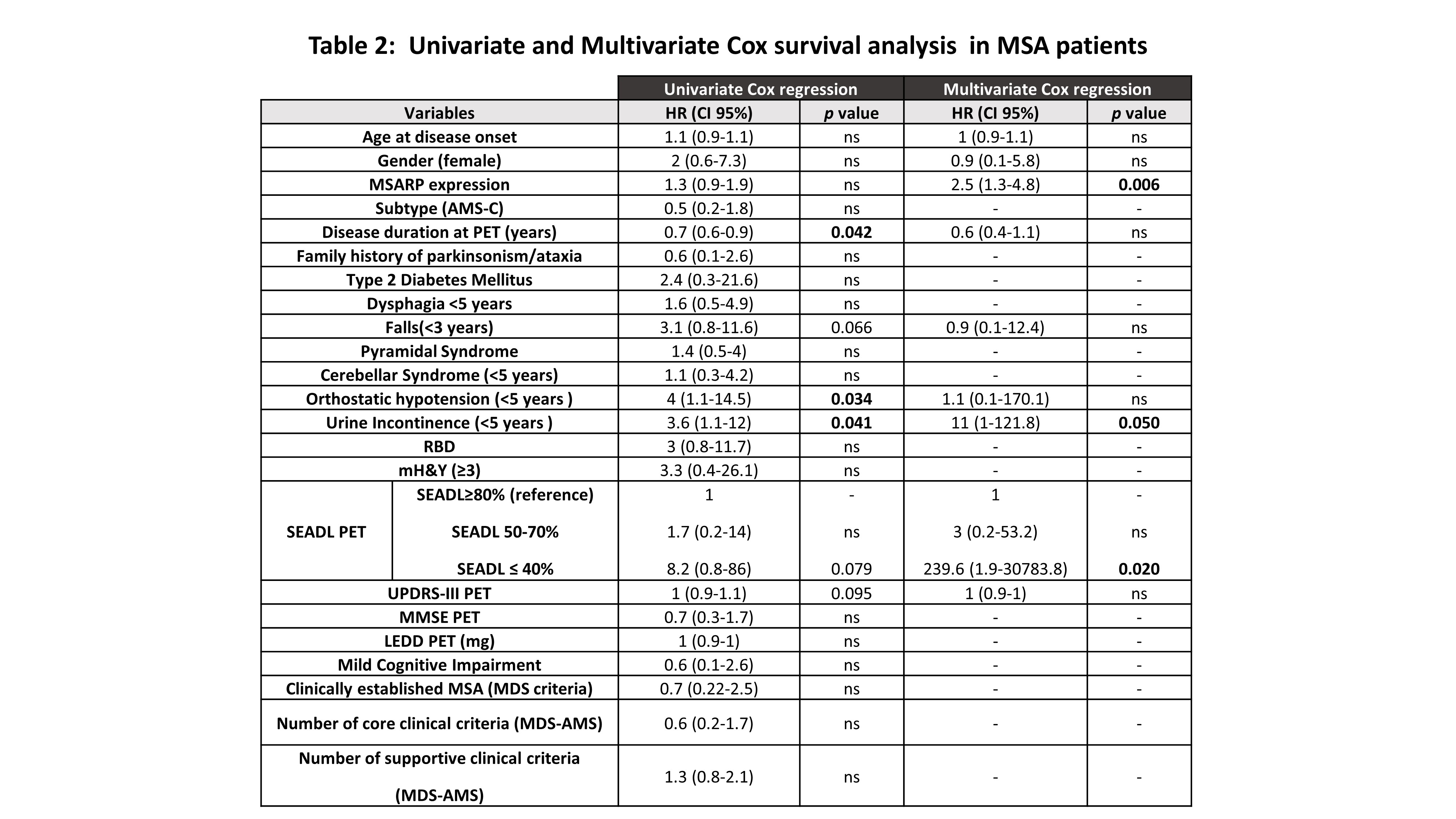
Method: We performed a retrospective longitudinal cohort study and included a total of 47 MSA patients who had been referred for an FDG-PET scan throughout the disease course . We performed a systematic review of medical records and obtained clinical and neuroimaging variables, including the date of death or last follow-up visit date in subjects who were alive in December 2022. We included the individual expression of a predefined MSA-related pattern (MSARP)5 obtained using a multivariate Scaled Subprofile Model/Principal Component Analysis (SSM/PCA) into FDG-PET scans. A Kaplan-Meier test was performed to calculate the median of survival. The risk of death in MSA patients was calculated using a Cox proportional hazard model in univariate analysis. We also selected variables that had previously been identified as predictors of survival and/or variables with biological plausibility. Those variables were entered into the multivariate Cox regression model.
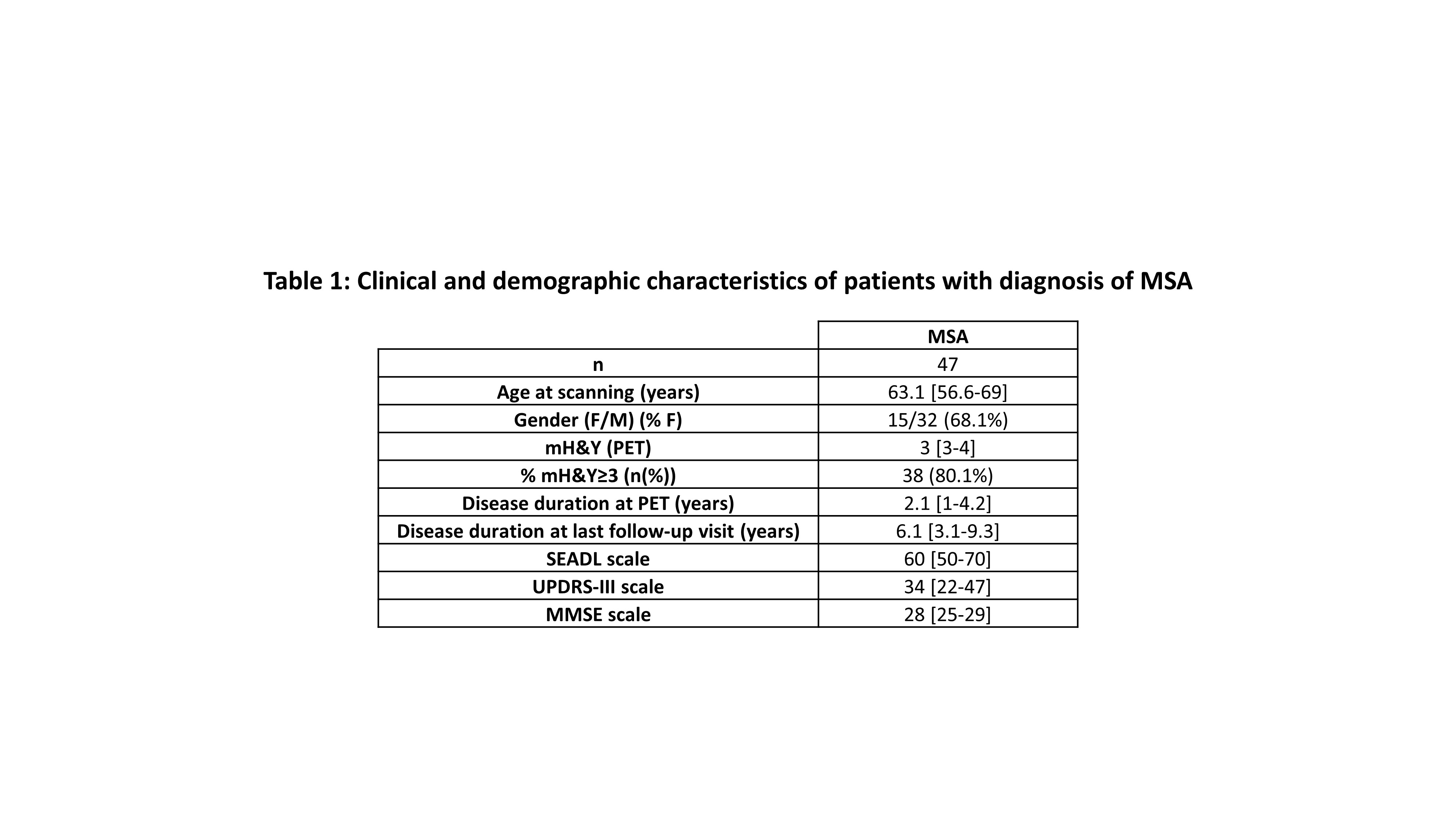
Results: Clinical variables are described in [Table1]. MSA patients were followed up for a median of 6.1 years and a total of 15 MSA patients died (MSA-P n=9, MSA-C n =6). The median overall survival was 10.6 [8.5-14.1] years, and we did not find differences in survival between subtypes (MSA-P 9.8 [9.3-11.3] years, and MSA-C 12 [6.6-15.8] years, p=0.911). The presence of early urinary incontinence (within the first five years of disease), a poor functional disability (SEADL<40%) at scanning, and a higher PET-FDG MSARP expression were independent risk factors of mortality [Table 2].
Conclusion: An early urinary incontinence, poor functional disability, and a more extensive MSA typical neuronal network dysfunction (MSARP expression) have a negative impact on survival.
Clinicalcs of patients with diagnosis of MSA
Survival analysis in MSA patients
References: 1. Cao B, Zhang L, Zou Y, et al. Survival analysis and prognostic nomogram model for multiple system atrophy [Internet]. Park. Relat. Disord. 2018;54(February):68–73.Available from: https://doi.org/10.1016/j.parkreldis.2018.04.016
2. Glasmacher SA, Leigh PN, Saha RA. Predictors of survival in progressive supranuclear palsy and multiple system atrophy: a systematic review and meta-analysis [Internet]. J. Neurol. Neurosurg. Psychiatry 2017;88(5):402–411.Available from: https://jnnp.bmj.com/lookup/doi/10.1136/jnnp-2016-314956
3. Du J, Cui S, Huang P, et al. Predicting the Prognosis of Multiple System Atrophy Using Cluster and Principal Component Analysis [Internet]. J. Parkinsons. Dis. 2023;13(6):937–946.Available from: https://www.medra.org/servlet/aliasResolver?alias=iospress&doi=10.3233/JPD-225127
4. Eschlboeck S, Goebel G, Eckhardt C, et al. Development and Validation of a Prognostic Model to Predict Overall Survival in Multiple System Atrophy. 2023;10(June):1368–1376.
5. Martí-Andrés,G.,etal. Abnormal pattern of brain glucose metabolism in multiple system atrophy. 25th International Congress of Parkinson ́s Disease and Movement Disorders. MDS virtual congress 2020.
To cite this abstract in AMA style:
G. Martí-Andrés, E. Prieto-Azcárate, CA. Espinoza-Vinces, M. Riverol, J. Arbizu, MR. Luquin-Puido. Clinical and neuroimaging factors associated with survival in Multiple System Atrophy [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/clinical-and-neuroimaging-factors-associated-with-survival-in-multiple-system-atrophy/. Accessed July 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-and-neuroimaging-factors-associated-with-survival-in-multiple-system-atrophy/