Session Information
Date: Saturday, October 6, 2018
Session Title: Surgical Therapy: Parkinson's Disease
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: To describe the DBS practice patterns at University of Miami Movement Disorder Center, motor outcomes and health disparities among ethnic groups.
Background: Deep brain stimulation (DBS) improves motor outcomes and quality of life in Parkinson’s disease (PD) patients (1,2). However, few studies have examined referral patterns for deep brain stimulation (DBS) patients from multi-ethnic communities(3,4).
Methods: Retrospective chart review from the University of Miami DBS referred patients.
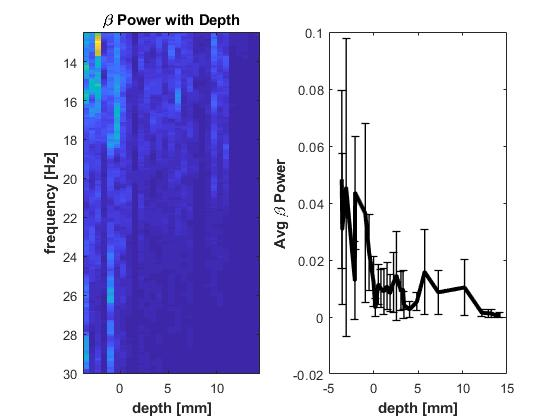
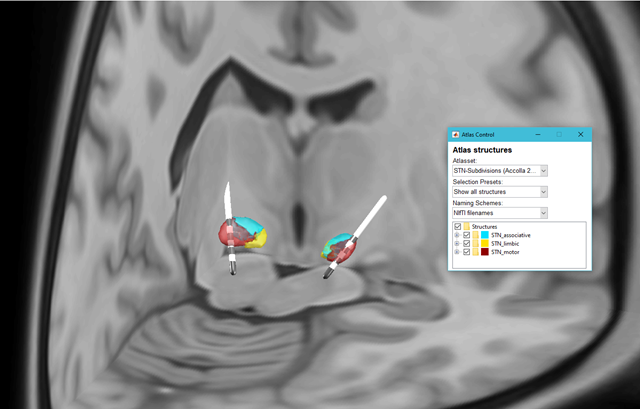
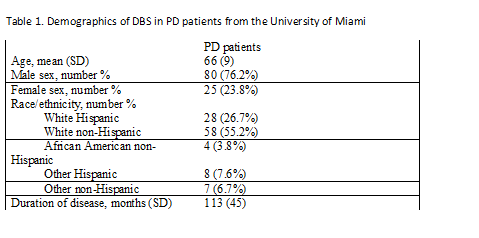
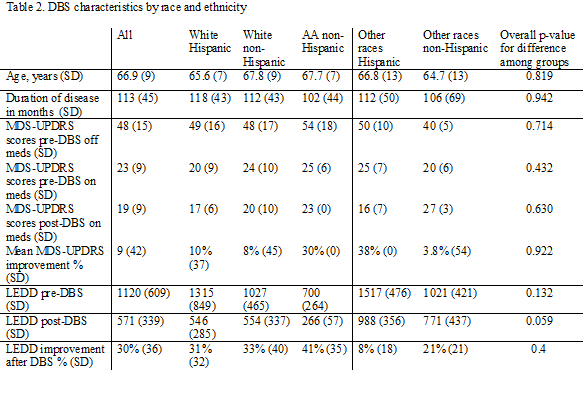
Results: From January 2014 to September 2017, 3609 patients with PD were evaluated at the University of Miami Movement Disorders Center. 1363 patients were female and 2245 male. 2832 of the PD patients seen in our facility were white, 142 African American, 28 Asian, 290 multiracial and 303 unknown. In total, 201 PD patients have been referred for DBS surgery from January, 2014 to July, 2017. From these, 99 (84%) were considered white, 3 (1.5%) African Americans. The average age was 65(+/-9) and mean disease duration when referred to DBS was 9.4(+/-3.7) years [table1]. 32.8 % had uncontrolled motor fluctuations, 17% poorly controlled tremors and 3% freezing of gait as the reason for referral. After multidisciplinary team evaluation, 106 patients (51%) underwent BL STN DBS or GPI DBS. The mean MDS-UPDRS score pre-DBS off medications was 49(+/-16), on meds was 23(+/-10). Stereotactical planning was performed using WayPoint Navigator software and and postoperative lead placement confirmation was done using LEAD-DBS [figure1]. Local field potentials were recorded from each individual electrode pass and beta power was calculated using in house developed software[figure2]. At 12 months after the surgery the motor score improved 59.2% (DBS ON, MEDS ON= 20+/-9) with DBS ON, meds OFF mean MDS UPDRS was 24 +/- 14 (51.1%). Patients also reported an overall decrease in levodopa equivalent daily dose (LEDD) from 1120 (+/609) to 572 (+/-339), 49% reduction[table 2]. One patient had hemorrhage that was managed conservatively, and one infection required IPG exchange.
Conclusions: Significant improvement in motor UPDRS and decrease in medication after DBS was seen across all ethnic groups. In Miami, the referral pattern includes mostly the white population despite the majority Hispanic and African American population. Efforts should be made to better identify this disparities, to develop national multicenter data collection registries and to develop best practice guidelines in order to improve outcomes.
References: 1. Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, et al. A Randomized Trial of Deep-Brain Stimulation for Parkinson’s Disease. N Engl J Med. 2006 Aug 31;355(9):896–908. 2. Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ, et al. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA. 2009 Jan 7;301(1):63–73. 3. Willis AW, Schootman M, Kung N, Wang X-Y, Perlmutter JS, Racette BA. Disparities in deep brain stimulation surgery among insured elders with Parkinson disease. Neurology. 2014 Jan 14;82(2):163–71. 4. Chan AK, McGovern RA, Brown LT, Sheehy JP, Zacharia BE, Mikell CB, et al. Disparities in access to deep brain stimulation surgery for Parkinson disease: interaction between African American race and Medicaid use. JAMA Neurol. 2014 Mar;71(3):291–9.
To cite this abstract in AMA style:
C. Luca, D. Garbin diLuca, H. Moore, C. Singer, I. Cajigas, J. Jagid. Practice patterns, motor outcomes and health disparities in patients undergoing Deep Brain Stimulation for Parkinson’s disease [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/practice-patterns-motor-outcomes-and-health-disparities-in-patients-undergoing-deep-brain-stimulation-for-parkinsons-disease/. Accessed July 3, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/practice-patterns-motor-outcomes-and-health-disparities-in-patients-undergoing-deep-brain-stimulation-for-parkinsons-disease/